Microbiome and Host Response Signatures for Pneumonia Among Lung Transplant Recipients
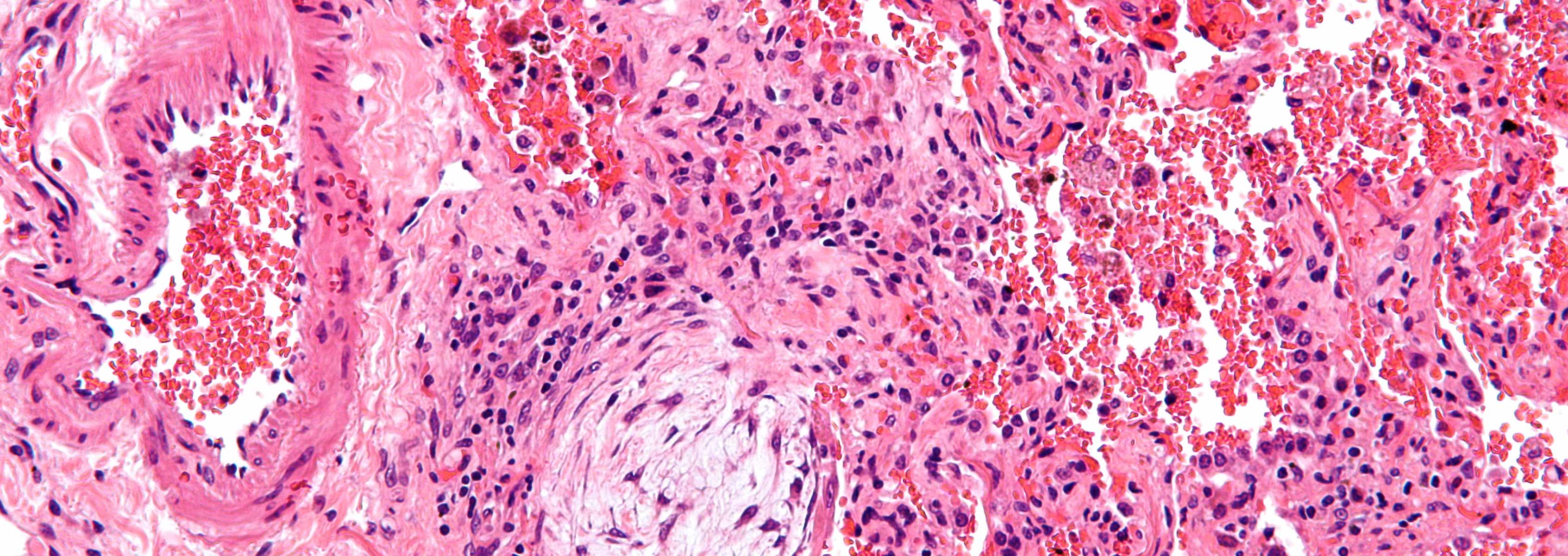
Pneumonia is a leading cause of death following lung transplantation. Guidelines endorse a diagnosis of tracheobronchitis rather than pneumonia for lung transplant recipients with signs and symptoms consistent with respiratory tract infection and positive cultures, and in whom there are no new or progressive lung parenchymal findings. However, conclusive pathologic evidence for tracheobronchitis among lung transplant recipients is lacking, and it is unclear if this diagnosis constitutes a coherent disease entity. Since diagnostic criteria for pneumonia and tracheobronchitis following lung transplantation are non-specific, it is often difficult to distinguish respiratory tract infections from colonization in the absence of disease or from non-infectious conditions like acute cellular rejection or chronic rejection due to bronchiolitis obliterans syndrome. Respiratory tract cultures may be positive with each of these diseases.
DNA sequencing-based microbiome profiling studies have demonstrated that the lower respiratory tract harbors complex microbial populations. Recent data indicate that pneumonia is characterized by loss of microbial diversity and emergence of a dominant pathogen. Specific members of the lung microbiota have been shown to stimulate discrete immune cell populations, and to correlate with general indicators of inflammation in lung transplant and non-lung transplant populations. Microbiome and inflammatory markers that distinguish between pneumonia, tracheobronchitis and respiratory tract colonization are undefined.
In collaboration with Drs. Neal Clancy and Hong Nguyen and the University of Pittsburgh Medical Center the long-term research objectives are to apply an understanding of the pathogenesis of respiratory tract infections to devise better diagnostic and management strategies.
The primary goal of the study is to refine and validate the multivariable signatures we detected for pneumonia, tracheobronchitis and respiratory tract colonization among lung transplant recipients. Specific focus will be on identifying microbiome and cytokine signatures of pneumonia, tracheobronchitis and colonization in lung transplant recipients and validating microbiome and cytokine signatures of pneumonia, tracheobronchitis and colonization in lung transplant recipients.
We anticipate that this study will define optimized, non-culture-based, disease-specific signatures for these three important diagnoses. The project is expected to lead to multi-center trials validating the signatures, and to studies in settings outside of lung transplantation, such as ventilator-associated pneumonia or tracheobronchitis. Furthermore, our results will provide insights into possible pathogenic mechanisms for the underlying diseases, which can inform subsequent mechanistic studies. A particularly important outcome of this study will be a deeper understanding of whether tracheobronchitis, as currently defined, constitutes a true infectious disease or an inflammatory state associated with complex respiratory tract ecosystem dysbiosis.
The Nierman Team will aid in determining the lower respiratory tract microbiome composition from bronchoalveolar lavage samples.
Funding
National Institutes of Health (NIH) funding provided through a subcontract from the University of Pittsburgh.