Understanding Dissemination Routes of Antibiotic Resistance During Early Life
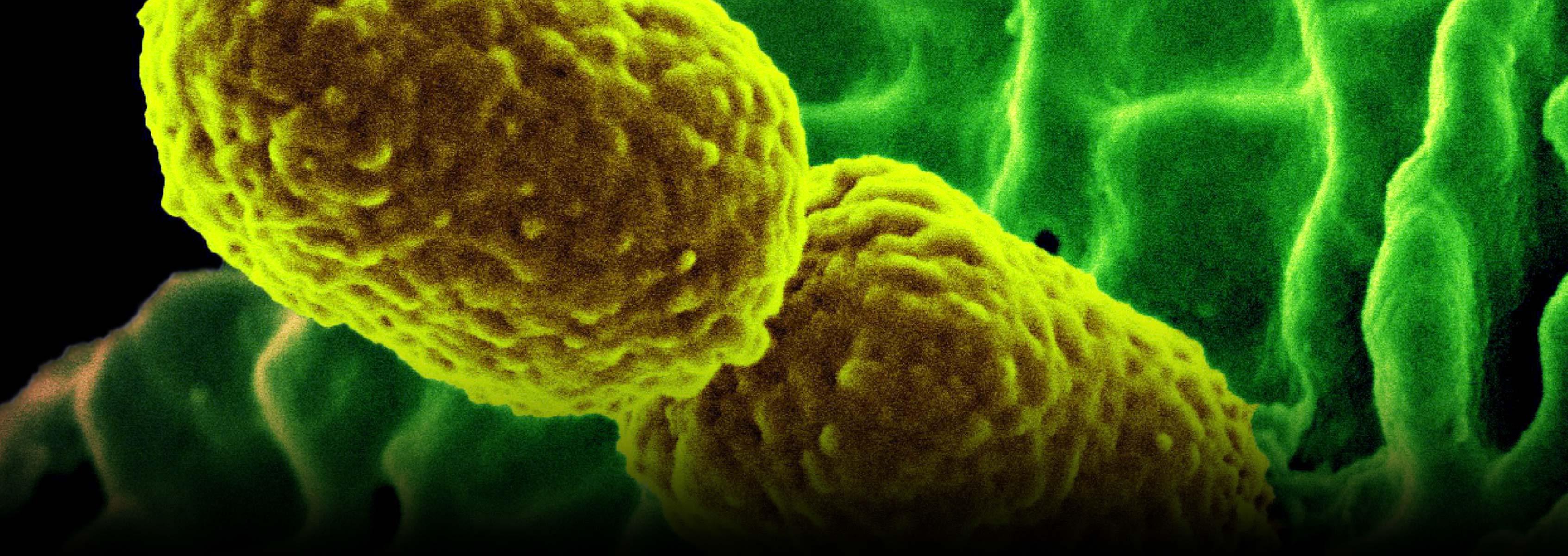
Antimicrobial resistance (AMR) is a global health concern of increasing magnitude. The selective pressure driven by the use and misuse of antimicrobials as prescribed in clinical medicine in humans and in the prevention, control, and treatment of disease in food-producing animals, as well as the transmission of resistant microbes from person to person and the transmission of AMR elements across microbes within individual patients are among the major forces influencing the spread of AMR. As new resistance mechanisms emerge and spread globally, our ability to manage infectious diseases in humans is increasingly threatened. In addition, due to constant seeding from, and exposure to, the environment, the human microbiome is particularly susceptible to becoming reservoirs for AMR.
The newborn and infant microbiome is strongly shaped by seeding from the maternal birth canal and maternal skin (mode of delivery), the surrounding primal environment, and food stimuli. Recent studies suggest that the spread of AMR may begin during this critical stage of development. Some reports imply that AMR elements may be present in the microbiome even before birth, and that antibiotic stimuli after birth may further impact the microbiome in the first years of life and primary care stages. Other reports suggest that the AMR elements present in the infant microbiome are unique and different from that of the mothers, suggesting that early environmental determinants (different from maternal ones) may shape AMR development in the infant. Environments, such as treatment in neonatal or pediatric intensive care units could be an alternative route of AMR transmission in newborns. Antibiotic exposure in early infancy has been associated with increased occurrence of diseases such as obesity, diabetes, allergies, and asthma.
This study seeks to characterize the microbiome of newborns exposed to antibiotics, paired with AMR elements identified in the microbiome of the mother and microbiome of neighboring NICU/maternity ward infants, to identify dissemination routes of AMR in the early infant microbiome, be they vertically passed from the mother, or horizontally passed from nearby infants in the hospital. The route of AMR dissemination in newborn infants, and those in intensive care units must be understood in order to design ways to limit transmission of AMR, such as improving the structure of hospital wards and focusing antimicrobial prophylaxis during delivery and treatment after birth.
Funding
This project is currently seeking a funding partner. Please contact the JCVI Development Office at development@jcvi.org to learn more.